New (2014) AHA/ACC Guideline for Management of Valvular Heart Disease
New, 2014 AHA/ACC, Guideline for the Management of Patients With Valvular Heart Disease: has been released. This document is a major revision of the 2006 and 2008 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines on the management of patients with valvular heart disease. There are substantial changes in multiple areas, and practitioners who are involved in the care of patients with heart valve disease should read at least the executive summary, if not the full guideline document.
The following are 10 areas with important changes to remember:
1. Stages of heart valve disease. The revised guidelines include a new classification of heart valve diseases with four progressive stages: A, at risk; B, progressive; C, asymptomatic severe; and D, symptomatic severe. For each valve lesion, stages are based on valve anatomy, valve hemodynamics, hemodynamic consequences, and symptoms.
2. The heart valve team. The guidelines recommend (Class I) that the management of patients with severe heart valve disease is best achieved by a heart valve team, composed minimally of a cardiologist and a cardiac surgeon; but potentially including cardiologists, structural valve interventionalists, cardiovascular imaging specialists, cardiovascular surgeons, anesthesiologists, and nurses, all of whom have expertise in the management and outcome of patients with severe heart valve disease.
3. Heart valve centers of excellence. The guidelines recommend (Class IIa) that consultation with or referral to a heart valve center of excellence is reasonable for asymptomatic patients with severe valve disease, patients with disease that could be best treated with valve repair rather than replacement, and patients with multiple comorbidities in whom valve intervention is considered. Specific criteria for a heart valve center of excellence include experienced providers from multiple disciplines, an ability to offer all available options for diagnosis and management, participation in regional or national outcome registries, demonstrated adherence to guidelines, ongoing quality improvement processes, and public reporting of intervention mortality and success rates.
4. Evaluation of surgical and interventional risk. The guidelines provide specific recommendations for the assessment of surgical and interventional risks that include the Society of Thoracic Surgeons (STS) predicted risk of mortality (PROM) calculator, patient frailty (e.g., Katz Activities of Daily Living and independence), the number of compromised major organ systems, and procedure-specific impediments.
5. Exercise testing. The guidelines place increased emphasis (Class IIa) on the use of exercise testing in the evaluation of asymptomatic patients with severe heart valve disease (notably including asymptomatic severe aortic stenosis [AS] and asymptomatic severe primary mitral regurgitation [MR]); aimed at confirmation of the absence of symptoms, assessment of the hemodynamic response to exercise, and assessment of prognosis.
6. Aortic stenosis. Changes were made in the characterization of and indications for intervention for AS:
- Two important changes were made in the characterization of AS:
i) ‘very severe’ AS is defined as aortic Vmax ≥5 m/s or mean gradient ≥60 mm Hg; and
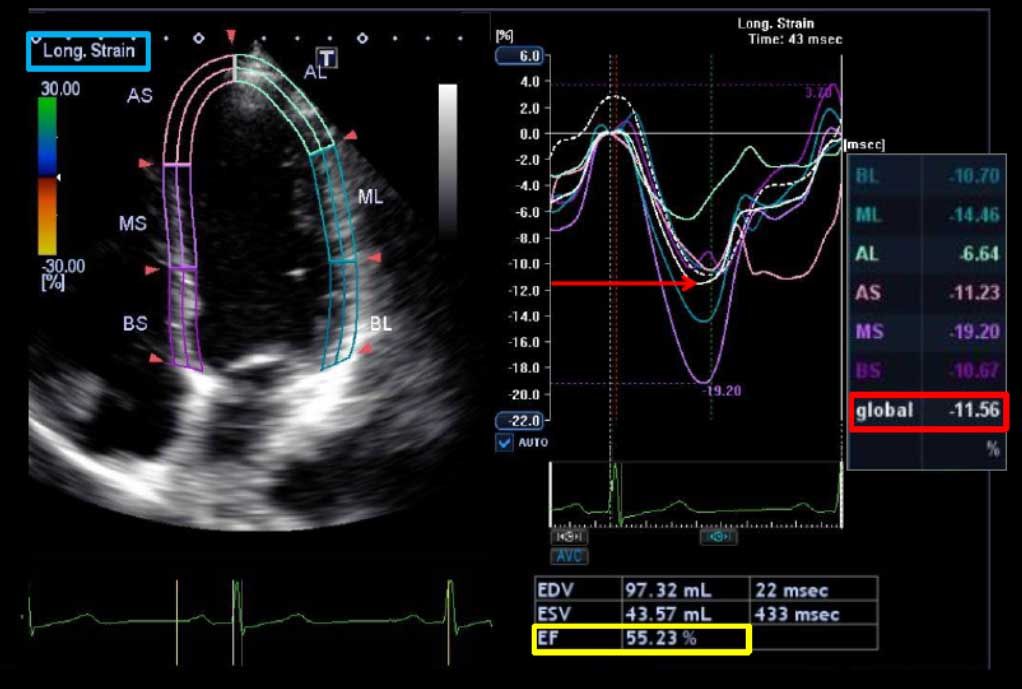
ii) symptomatic severe AS is subdivided into high gradient (Vmax ≥4 m/s or mean gradient ≥40 mm Hg), low-flow low-gradient (LFLG) with reduced left ventricular ejection fraction (LVEF) (severe leaflet calcification with severely reduced motion, effective orifice area [EOA] ≤1.0 cm2, and Vmax <4 m/s or gradient <40 mm Hg with LVEF <50%, and EOA remaining ≤1.0 cm2, but Vmax ≥4 m/s at any flow rate during dobutamine echocardiography), and LFLG with normal LVEF (or paradoxical LFLG severe AS; severe leaflet calcification with severely reduced motion, EOA ≤1.0 cm2 and Vmax <4 m/s or gradient <40 mm Hg with LVEF ≥50%).
- Indications for intervention are expanded from previous to include patients with very severe AS (above) and low surgical risk (Class IIa); asymptomatic severe AS and decreased exercise tolerance or exercise-related decrease in blood pressure (Class IIa); and symptomatic patients with LFLG severe AS and normal LVEF if clinical, hemodynamic, and anatomic data support valve obstruction as the likely cause of symptoms (Class IIa).
7. Transcatheter aortic valve replacement. Surgical aortic valve replacement (AVR) remains the intervention of choice for patients with an indication for AVR and low or intermediate operative risk (Class I). Transcatheter AVR (TAVR) is recommended for patients with an indication for AVR, but a prohibitive surgical risk (Class I). TAVR is a reasonable alternative to surgical AVR in patients with an indication for AVR and high surgical risk (Class IIa). Notably, members of a heart valve team should collaborate in order to optimize patient care for patients in whom TAVR or high-risk surgical AVR are being considered (Class I).
8. Management of primary MR. A clear distinction is drawn between chronic primary (degenerative) MR, with pathology of one or more components of the valve (leaflets, annulus, chordae, papillary muscles); and chronic secondary (functional) MR. Intervention for severe chronic primary MR remains indicated (all Class I) for symptoms, LV dysfunction (LVEF ≤60% and/or systolic diameter ≥40 mm), and at the time of other cardiac surgical intervention. Changes in the recommendations for mitral valve repair (MVr) include the following:
- MVr is recommended over mitral valve replacement (MVR) when pathology is limited to the posterior leaflet (Class I);
- MVr is recommended over MVR when pathology involves the anterior or both leaflets and a successful and durable repair can be accomplished (Class I);
- ‘Prophylactic’ MVr (repair in an asymptomatic patient with preserved LV function) is reasonable when performed at a heart valve center of excellence and the likelihood of successful and durable repair without residual MR is >95% and operative mortality risk is <1% (Class IIa);
- MVr is reasonable in an asymptomatic patient with severe nonrheumatic MR and preserved LV function in the setting of new-onset atrial fibrillation or resting pulmonary artery systolic pressure >50 mm Hg (Class IIa); and
- MVr may be considered in the setting of rheumatic mitral valve disease when surgery is indicated and either successful repair is likely or when long-term anticoagulation management appears unreliable (Class IIb). There is a Class III (harm) indication for MVR in the setting of isolated disease involving less than half of the posterior mitral leaflet unless repair was attempted and was unsuccessful.
- Finally, transcatheter MVr may be considered in severely symptomatic patients who have favorable anatomy and a reasonable life expectancy and a prohibitive surgical risk due to comorbidities, and remain severely symptomatic despite optimal medical therapy (Class IIb).
9. Management of secondary MR. Chronic secondary (functional) MR occurs as a result of abnormalities of the LV, and has more differences than similarities with chronic primary MR (above). The treatment of chronic secondary MR involves treatment of the underlying cardiomyopathy (Class I) and cardiac resynchronization therapy if indicated (Class I). Intervention for chronic secondary MR is reasonable at the time of coronary artery bypass grafting or other cardiac surgery if MR is severe (Class IIa) and not unreasonable if MR is moderate (Class IIb). Surgical intervention performed primarily for chronic secondary MR remains limited to severely (New York Heart Association class III-IV) symptomatic patients with persistent symptoms despite optimal medical therapy for heart failure (Class IIb); new in these guidelines is acceptance of equivalence among these patients between MVR and MVr.
10. Low molecular weight heparin (LMWH) ‘bridging’ of patients with a mechanical heart valve prosthesis. Low LMWH ‘bridging’ is now considered to be appropriate (Class I) among patients with a mechanical valve at high risk of thrombosis when warfarin needs to be interrupted in the context of an invasive or surgical procedure (previously Class IIb).
Source: D.S. Bach, MD (Cardiosource)