European Society of Cardiology (ESC) Guidelines on the management of valvular heart disease (version 2012)
A great number of guidelines have been issued in recent years by the European Society of Cardiology (ESC) as well as by other societies and organizations. Because of their impact on clinical practice, quality criteria for the development of guidelines have been established, in order to make all decisions transparent to the user.
The first step of evaluation of patients with valvular heart disease begins by obtaining a good clinical history. The aim of obtaining a case history is to assess symptoms and to evaluate for associated comorbidity. Essential questions in the evaluation of a patient for valvular intervention should include the following:
• Is valvular heart disease severe?
• Does the patient have symptoms?
• Are symptoms related to valvular disease?
• What are patient life expectancy and expected quality of life?
• Do the expected benefits of intervention (vs. spontaneous outcome) outweigh its risks?
• What are the patient’s wishes?
• Are local resources optimal for planned intervention?
The following are 10 points to remember about these new ESC guidelines on the management of valvular heart disease (VHD):
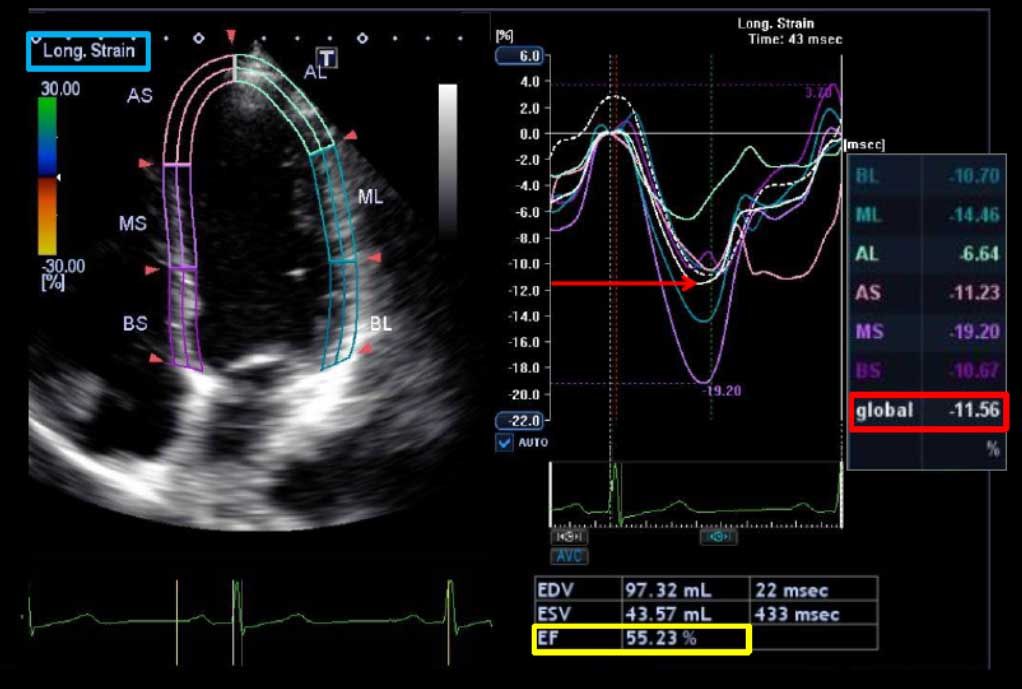
1. Echocardiography is the key technique used to confirm the diagnosis of VHD, as well as to assess its severity and prognosis. It is indicated in any patient with a murmur, unless no suspicion of valve disease is raised after the clinical evaluation. Transesophageal echocardiography should be considered when transthoracic echocardiography is of suboptimal quality or when thrombosis, prosthetic dysfunction, or endocarditis is suspected.
2. Exercise Stress Testing: The primary purpose of exercise testing is to unmask the objective occurrence of symptoms in patients who claim to be asymptomatic or have doubtful symptoms. Exercise testing has an additional value for risk stratification in AS. Exercise testing will also determine the level of authorized physical activity, including participation in sports. The use of stress tests to detect coronary artery disease (CAD) associated with severe VHD is discouraged because of their low diagnostic value and potential risks.
Exercise echocardiography may provide additional information in order to better identify the cardiac origin of dyspnea—which is a rather unspecific symptom—by showing, for example, an increase in the degree of mitral regurgitation/aortic gradient and in systolic pulmonary pressures.
3. Coronary angiography is recommended before valve surgery in patients with severe VHD and any of the following: history of CAD; suspected myocardial ischemia; left ventricular (LV) systolic dysfunction; in men aged over 40 years and postmenopausal women; and ≥1 cardiovascular risk factor.
Coronary angiography can be omitted in young patients with no atherosclerotic risk factors (men <40 years and premenopausal women) and in rare circumstances when its risk outweighs benefit, e.g. in acute aortic dissection, a large aortic vegetation in front of the coronary ostia, or occlusive prosthetic thrombosis leading to an unstable hemodynamic condition.
4. In severe aortic regurgitation, surgery is indicated in symptomatic patients, in asymptomatic patients with resting LV ejection fraction (LVEF) ≤50%, and in patients undergoing coronary artery bypass grafting (CABG) or surgery of ascending aorta, or on another valve.
5. Aortic valve replacement is indicated in patients with severe aortic stenosis (AS) and any symptoms related to AS, in patients with severe AS undergoing CABG, surgery of the ascending aorta or another valve, in asymptomatic patients with severe AS and systolic LV dysfunction (LVEF <50%) not due to another cause, and in patients with severe AS and abnormal exercise test showing symptoms on exercise clearly related to AS.
6. Transcatheter aortic valve implantation (TAVI) should only be undertaken with a multidisciplinary ‘heart team’ including cardiologists and cardiac surgeons and other specialists if necessary, and should only be performed in hospitals with cardiac surgery on-site.
7. TAVI is indicated in patients with severe symptomatic AS who are not suitable for AVR as assessed by a ‘heart team,’ and who are likely to gain improvement in their quality of life, and to have a life expectancy of more than 1 year after consideration of their comorbidities.
8. In severe primary mitral regurgitation, mitral valve repair should be the preferred technique when it is expected to be durable. Surgery is indicated in symptomatic mitral regurgitation patients with LVEF >30% and LV end-systolic dimension (LVESD) <55 mm and in asymptomatic patients with LV dysfunction (LVESD ≥45 mm and/or LVEF ≤60%).
9. Percutaneous mitral commissurotomy is indicated in symptomatic mitral stenosis patients with favorable characteristics, and in symptomatic patients with contraindication or high risk for surgery.
10. For valve replacement, a mechanical prosthesis is recommended according to the desire of the informed patient and if there are no contraindications for long-term anticoagulation, and a bioprosthesis is recommended when good quality anticoagulation is unlikely (compliance problems; not readily available) or contraindicated because of high bleeding risk (e.g., prior major bleed, comorbidities, unwillingness, compliance problems, lifestyle, occupation).
Source: 1)- Vahnnian A, et al. Eur heart J 2012; 33:2451-2496; 2)- Mukherjee D.: Cardiosource.