Electrical Cardioversion
Electrical Cardioversion is a procedure carried out to restore a normal cardiac rhythm in selected patients whose heart rhythm is abnormal. It involves the controlled delivery of energy through the chest wall in order to “electrically reset” the heart. Most scheduled cardioversions are done for patients with atrial fibrillation (AF) or atrial flutter (AFL). Sometimes, though, cardioversions may be carried out for supraventricular tachycardia (SVT) or the stable form of ventricular tachycardia (VT).
Cardioversions are slightly different from defibrillation. While both procedures involve delivering a shock to the heart, defibrillation is usually carried out for immediately life threatening arrhythmias like ventricular fibrillation (VF). Cardioversions are generally done in non-urgent situations, and are, in fact, often scheduled procedures. Some are done in Emergency Departments, and others may be done in Electrophysiology (EP) Labs.
How is electrical cardioversion done?
Electrical cardioversion is carried out with either deep sedation or general anesthesia. Patients have an IV placed in their hand or wrist, and medication is administered to allow the patient to drift off to sleep. Sticky pads are placed on the chest and back, and hooked up to an external defibrillator. (Sticky pads are now used instead of “the paddles” that most people are familiar with from TV shows). When the patient is asleep, the physician delivers a shock (ranging from 50-360 Joules, depending on the arrhythmia and other factors like patient size). Usually, only one shock is required. However, if the first shock does not work, the physician may elect to try 2-3 more times with higher energies, or with the sticky pads in a different place.
Usually, the procedure is over within minutes, and patients recover quickly.

A defibrillator, used for electrical cardioversions
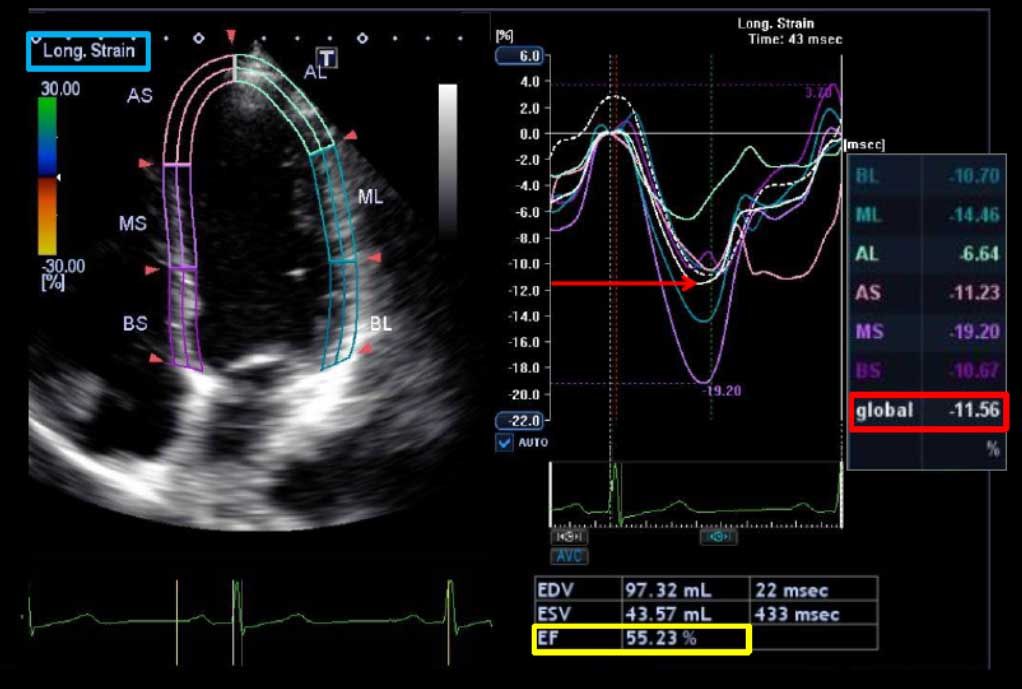
An ECG Before, During, and After Cardioversion for Atrial Fibrillation (AF)
What are the chances that electrical cardioversion will work for me?
The chances that cardioversion will successfully restore the normal rhythm for you depends on many factors, including the arrhythmia you have, how long you have been in it, the size of your heart chambers, medications you are on, and other factors. Your doctor will discuss this with you.
What are the risks of electrical cardioversion?
Cardioversion is generally considered to be a low-risk procedure.
Some patients will describe a burning sensation of the skin for a few days afterwards (like a sunburn), but this is usually self-limiting.
Rare complications, like heart failure or stroke, have been reported.
Your doctor will discuss the risks with you as they vary depending on the specific condition you have.
What about blood thinners?
Some arrhythmias, like atrial fibrillation (AF) and atrial flutter (AFL) ordinarily require blood thinners (like coumadin or warfarin) to be taken before and after a cardioversion. This is because these arrhythmias are associated with an elevated risk of stroke, and being on blood thinners helps to reduce that risk. Restoring the normal rhythm sometimes results in a few days of sluggish blood flow in the upper chambers of the heart (the atria), and this can therefore be a higher risk period for stroke. This is why it is extremely important to be on adequate doses of blood thinners before, during, and after the cardioversion.
Some patients, though, can’t take blood thinners, but still need a cardioversion. Others need a cardioversion, but can’t wait for three weeks for blood thinners to “kick in”. In these special cases, a special test called a transesophageal echocardiogram (TEE) may be arranged by your doctor. This is a test that allows for imaging of the upper chambers of the heart, particularly the left atrium, where blood clots tend to form. A tube with an ultrasound probe is passed down the swallowing tube (the esophagus), and pictures are taken. If there is no clot, the cardioversion may be able to go ahead even without blood thinners on board.
What else should I know about electrical cardioversion?
- You should have nothing to eat or drink for at least eight hours prior to the procedure.
- Take your regularly scheduled medications the morning of the procedure unless your doctor has told you otherwise. Your medications should only be taken with enough water to get the tablets down. If you are diabetic, you should discuss your insulin or other diabetes medication dosing with your doctor.
- Bring a list of all your medications with you.
- Most centers will not let you drive yourself home after receiving anesthesia; therefore you should arrange a ride home that day.
- For the remainder of the day, you should not operate a car, drink alcohol, operate heavy machinery, or make any important decisions.
Don’t stop blood thinners (e.g. warfarin, coumadin) after the cardioversion until your doctor tells you that you can.