New guidance for management of asymptomatic young people with Wolff-Parkinson-White (WPW) syndrome
A consensus statement on the management of asymptomatic patients with Wolff-Parkinson-White (WPW) syndrome has been presented at The Heart Rhythm Society (HRS) 2012 Scientific Sessions. This statement should help clarify which young people should undergo catheter ablation. While there is a small chance that an asymptomatic young person could end up having a life-threatening arrhythmia, the number is not zero. Yet, catheter ablation for every young individual who has ever had a WPW pattern on his/her electrocardiogram (ECG) is also not the answer.
Cohen and colleagues released the statement on May 18, 2012 at the Heart Rhythm Society Scientific Sessions.
The guidance is explicitly directed at physicians treating young patients with WPW and defines young people as between eight and 21. At the crux of the document is the question of just when physicians should intervene—and when they shouldn’t—in young people found, on ECGs, to have the signature electrocardiographic WPW pattern. These are increasingly important questions, given increased emphasis on pre-participation screeningfor sports in young people.
The expert consensus statement, a joint effort of the Pediatric and Congenital Electrophysiology Society (PACES) and the HRS, estimates that from one to three young people per 1000 likely have WPW, although many—around 65%—are asymptomatic.
The guideline writers recommend the following:
- If a child is old enough to comply, an exercise stress test to look for persistent preexcitation is “reasonable.” Clear loss of preexcitation at physiologic heart rates is associated with lower risk of sudden death due to accessory pathways.
- Where noninvasive testing shows persistent or uncertain loss of preexcitation, diagnostic transesophageal or intracardiac electrophysiology studies are warranted. Recommendations, based on test results, include ablation or continued awareness and observation for symptoms.
- Ablation is a “reasonable” consideration in young people with a shortest preexcited RR interval (SPERRI) <250 ms. Young people with SPERRI >250 ms are lower risk, and ablation may be deferred.
- Patients deemed low risk who subsequently develop symptoms like syncope or palpitations may be eligible for ablation.
- WPW in the setting of structural heart disease increases risk for both atrial tachycardia and atrioventricular (AV) reciprocating tachycardia. Patients can be considered for ablation.
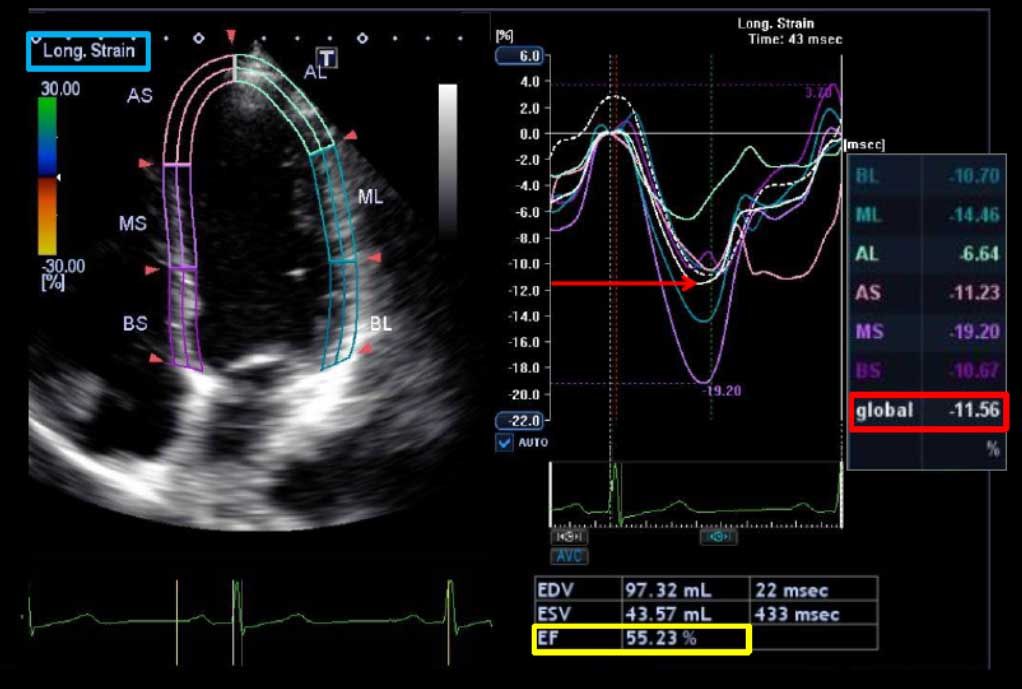
- Ablation may also be considered in asymptomatic patients with WPW who have ventricular dysfunction secondary to dyssynchronous contractions.
Source: The heart.org