Atrial Fibrillation
WHAT IS IT?
Atrial fibrillation (AF) is the most common heart rhythm disorder seen by doctors. It’s a big public health issue in terms of not only the sheer number of patients affected, but also by the fact that managing these specific arrhythmias (which is the medical name for heart rhythm problems) is expensive.
Also Known As: A Fib, AF, Atrial Fib, auricular fibrillation, supraventricular arrhythmia, supraventricular tachyarrhythmia
KEY FACTS
- In the United States, more than 2.2 million people have atrial fibrillation (AF) including 9% of people over the age of 80.
- About 15% to 20% of all strokes result from atrial fibrillation.
- AF can arise from temporary (acute) causes such as alcohol consumption, heart attack, surgery, lung disease, or a metabolic disorder (such as an overactive thyroid gland).
- AF can also be related to long-term (chronic) conditions such as high blood pressure, diabetes, or heart failure.
- Obesity is an important risk factor for the development of AF and weight loss may decrease the risk associated with AF.
- AF can be occasional (paroxysmal, which self terminates) or ongoing (persistent). If it does not respond to an electric current that is used to reset the heart’s rhythm back to its regular pattern (called cardioversion), it can progress to permanent AF.
- The most common signs of AF are heart palpitations, chest pain, and shortness of breath. AF can also be silent.
- There are two approaches to treatment: heart rate control or heart rhythm control, with therapies ideally achieving both goals.. When medication is ineffective, AF treatments can include cardioversion, ablation therapy (that targets specific cells that are causing the AF), and open-heart or minimally-invasive surgery that also targets a specific area of the heart that is causing the problem.
- Heart-healthy lifestyles can help prevent AF or make you better able to live with it.
BACKGROUND
The heart has an electrical system that controls both the speed and rhythm of each heartbeat. This electrical system is controlled by the autonomic nervous system, which also handles critical functions such as breathing and digestion – all those functions that need to happen automatically rather than under our conscious control.
When your heart beats, an electrical signal starts at the top of the heart in a group of cells called the sinus (or sinoatrial) node. This node, your heart’s natural pacemaker, is located in the right atrium, which is the upper right chamber of the heart. There are two atria (the right and left) and these function primarily as priming pumps for the two ventricles, the main squeezing chambers and workhorses of the heart.
The electrical signal from the sinus node travels through the right and left atrium to the atrioventricular (AV) node, a sort of relay station, where the electrical signal pauses before it spreads to the right and left ventricles. As the signal travels from the sinus node toward the AV node, it causes the atria to contract and pump blood into the ventricles, ensuring optimal filling of these chambers.
When the electrical signal then spreads from the AV node to the ventricles, it causes those chambers to squeeze, pushing blood out of the heart and into the body. This rhythmic, coordinated sequence of events ensures efficient heart function. A normal heart repeats this sequence automatically and without stopping, beating on average 60 to 100 times per minute. And when the electrical system is functioning normally, we say the patient is in “normal sinus rhythm”.
An arrhythmia occurs when the heart’s electrical system malfunctions causing a failure in the synchronization that’s required for the heart to work properly. In the specific arrhythmia known as atrial fibrillation, electrical signals no longer start in the sinus node, but rather fire rapidly and haphazardly throughout the heart’s upper chambers.
These disorganized electrical impulses cause the atria to contract quickly and irregularly, resulting in rapid quivering of the upper chambers, which is medically known as fibrillation (hence, the name atrial fibrillation). These chaotic and rapid electrical signals also bombard the AV node, usually causing heart rate to rise. As a result, the organized flow of blood within the heart becomes disrupted and heart rhythm becomes very irregular. It can also become quite fast, occasionally reaching heart rates as high as 160 beats per minute at rest.
Up to one-third of patients with atrial fibrillation have asymptomatic or “silent” AF, which is more common in the elderly. Other people with AF experience symptoms such as palpitations, fainting, chest pain, or even heart failure.
If the heart’s atria are not contracting properly, blood can pool in the heart’s upper chambers. Such pooled blood can lead to the formation of blood clots within the atria, which in turn can cause strokes if the clots are carried into the blood stream and lodge in the arteries of the brain.
AF is a major risk factor for stroke (increasing stroke risk about 5-fold) with the absolute level of risk somewhat dependent on the number of additional risk factors for stroke in a given individual. Just like there can be silent AF, strokes can be “silent” too, but even these asymptomatic strokes may have significant ramifications. For example, elderly people with silent strokes have greater than double the risk of dementia and a steeper decline in global cognitive function compared to age-matched individuals without evidence of such strokes.
One particular high-risk variable: transient ischemic attacks (TIAs). These are “warning strokes” that produce stroke-like symptoms but no lasting damage. A person who’s had one or more TIAs is almost 10 times more likely to have a stroke than someone of the same age and sex who hasn’t. Therefore a history of TIA and AF is a combination that suggests a strong need for preventive therapy and stroke risk reduction.
Patterns of AF
Doctors tend to label AF by its pattern of occurrence. Episodes that last 7 days or less (often less than 24 hours) are called “paroxysmal AF” and they usually stop on their own. However, when AF lasts longer than 7 days, it is considered “persistent” and may require treatment before the episode stops. When AF lasts longer than a year it is considered “permanent”. If an individual has two or more AF episodes, whether the arrhythmia stops on its own or must be stopped via therapy, the condition is considered “recurrent AF”.
BY THE NUMBERS
In the United States, about 2.2 million people have AF, and nearly 5 million are affected in the European Union. This is the most common arrhythmia that doctors see in practice, and AF is the cause of about one-third of all hospitalizations related to cardiac rhythm problems. Overall, hospitalizations for AF have increased 66% in the last 20 years. This is due to various factors, including the aging of the population, a rise in chronic heart disease, and more frequent diagnosis through the use of ambulatory monitoring devices. The annual cost per patient is approximately $3,600, which may not seem like a lot, but given how many people are afflicted with AF, that comes to well over $7 billion per year in the United States and about $15.7 billion per year in the European Union.
About 15% to 20% of all strokes occur in someone with AF, which in hard numbers means that AF causes about 70,000 strokes each year just in the United States alone. Stroke risk increases with age. While AF is seen in only about 1% of the total U.S. adult population, it affects about 3.8% of those older than 60 years and 9.0% of those older than 80 years. Up to 40% of patients with heart failure also experience AF, and patients with this combination of heart problems are at particularly high risk for cardiac death.
Approximately 30% to 45% of cases of paroxysmal AF (when the AF lasts for 7 days or less) and 20% to 25% of cases of persistent AF (that lasts for more than 7 days) occur in young patients without any identifiable underlying disease. This is known as “lone AF.”
CAUSES AND RISK FACTORS
Risk factors
There are several well-established risk factors for AF, with coronary artery disease and heart failure being most frequently associated with atrial fibrillation. Rheumatic heart disease, which affects the valves of the heart, and congenital heart abnormalities (inherited heart defects) also increase the chance of AF.
Cardiac risk factors such as hypertension and diabetes can also play a role in damaging the atria of the heart, leading to AF.
There are a number of acute, temporary causes of AF as well as chronic conditions which lead to this rhythm abnormality. For the most part, when the temporary condition ceases or is treated, AF usually resolves. In the presence of chronic conditions, treatment should target both the AF and the chronic problem that is contributing to the risk of AF-associated events.
Acute conditions
One acute condition associated with AF is excessive alcohol consumption. There is even a medical term for this: “holiday heart syndrome,” so named because the excessive consumption of alcohol that sometimes occurs with holiday celebrations is associated with a spike in the number of people presenting with AF.
Other acute conditions relate to medical factors such as surgery, lung disease, asthma attacks, extreme body stress due to conditions such as pneumonia, or the occurrence of a metabolic disorder, such as hyperthyroidism (overactive thyroid gland). An inflammation of the lining of the heart can also cause the atria to fibrillate, and having a heart attack increases the risk of AF.
Many of these acute conditions can cause chemical imbalances that can lead to electrical imbalances in your heart, triggering AF. Once the necessary balance is restored – for example, pneumonia resolves or alcohol is eliminated – the AF usually disappears on its own.
Chronic conditions
A number of chronic or long-term conditions also can lead to AF. For the most part, these consist of existing heart problems, such as congenital heart defects, particularly atrial septal defect, or heart valve diseases such as those related to prior rheumatic fever. These conditions tend to results in atrial enlargement, which in effect stretches out the electrical “wiring” of those chambers, making short circuits and sparks (AF) more likely. Additionally, AF may be associated with hypertrophic, dilated, or various other cardiomyopathies; these conditions also change the shape of the heart, interfering with the heart’s intricate electrical system. Longstanding lung problems such as COPD (chronic obstructive lung disease), can also predispose to atrial fibrillation.
Two other common conditions that can lead to AF are obesity and sleep apnea. In a study of more than 3,400 adult patients who never had atrial fibrillation, 14% ended up being diagnosed with AF after several years of follow-up. Beyond the typical risk factors mentioned above, the incidence of AF was strongly predicted both by obstructive sleep apnea and excess weight.
It turns out that obesity can actually change the size of the heart’s atria, with a graded increase in atrial size occurring as body weight increases from normal, to overweight, to obese. Weight loss has been shown to reduce atrial size, suggesting that weight reduction may decrease the risk of developing AF.
More than 25 million U.S. adults are estimated to have obstructive sleep apnea and the incidence of AF is about 5 times greater in people with apnea compared to people who do not have sleep apnea. Looking at it another way, between one third and one half of all patients with AF have sleep apnea.
Sleep apnea is a condition in which patients do not breathe normally or regularly during sleep. Instead, breathing pauses or becomes very shallow, with abnormal breathing episodes lasting a few seconds up to several minutes. These episodes can occur anywhere from 5 to 30 or more times per hour, disturbing restful sleep. This disrupted sleep can contribute to an increased risk of arrhythmias such as AF, although it is not clear whether this is due to biochemical alterations that occur when sleep is disrupted or other conditions that arise from sleep apnea.
Age and family history
AF tends to occur more frequently in older people, primarily because the older you are, the more likely you are to have heart disease or other health problems.
Although AF is often considered an electrical problem that is linked to underlying cardiac disease, that is not always the case. Approximately 30% to 45% of cases of paroxysmal AF and 20% to 25% of cases of persistent AF occur in younger patients who have no heart defects or disease (lone AF). The cause of lone AF may not be known for quite some time, if at all. When lone AF runs in a family, it is called familial AF. Your chances of developing AF are higher if your parents have or had it.
SIGNS AND SYMPTOMS
Probably the most recognizable sign of AF is heart palpitations, where your heart beats so fast that you think it is racing and/or you can feel it thumping or flopping in your chest. It may be accompanied by chest pain; lightheadedness or dizziness, especially if you are exerting yourself; weakness; or shortness of breath, including difficulty breathing when lying down. AF symptoms will vary depending on the degree of pulse irregularity and resultant heart rate, underlying functional status, how long the AF lasts, and individual patient factors.
Remember: one of the effects of AF may be formation of a blood clot in the atria. If this happens and the clot travels up to the brain, you may have a stroke. Sometimes a stroke is the first sign of underlying AF, especially if the symptoms have been light or nonexistent.
There is no set amount of time that marks an episode of AF – it may be very short and stop on its own or it may be prolonged and you find yourself in need of medical intervention. Over time, you may become more accustomed to the pattern of your AF, and what factors contribute to and relieve this arrhythmia.
TESTING AND DIAGNOSIS
First, your doctor will take a medical history from you looking for information on you and your family. The information from you will include questions that will: help your doctor understand your specific symptoms and how severe they may be; define your AF clinically (e.g., paroxysmal, persistent, or permanent); and reveal AF frequency, duration, precipitating factors, and how it terminated (if it did). If you received any treatment for the AF before seeing your doctor (if paramedics administered a drug or defibrillation therapy, for example), your doctor will want to review your response to such therapy. Finally, you will be examined to see if you have any heart disease that may be causing the AF or whether there may be a reversible condition, such as pneumonia, that triggered the AF.
Electrocardiograms and echocardiograms
You likely will have an electrocardiogram, known as an ECG or an EKG. This is a noninvasive test in which patches (called electrodes) are attached to your chest to detect and record the electrical activity of your heart. The electrical impulses travel by wires attached to the electrodes and are recorded as waves on a sheet of paper. This test allows your physician to see how fast your heart is beating and whether the rhythm is regular or irregular. A number of heart irregularities and conditions are detectable with an ECG. The tracing can even provide clues as to whether or not you have had a previous heart attack.
If you do not have AF at the time of your ECG – for instance, if you have paroxysmal AF and the episode has abated – then you may be asked to wear a portable or “ambulatory” ECG monitor. One type, a Holter monitor, records your heart’s activity continuously for a 24- or 48-hour period. Other devices, called “event monitors”, record only when you press a button to indicate that you are feeling symptoms. Event monitors can be worn for up to one month.
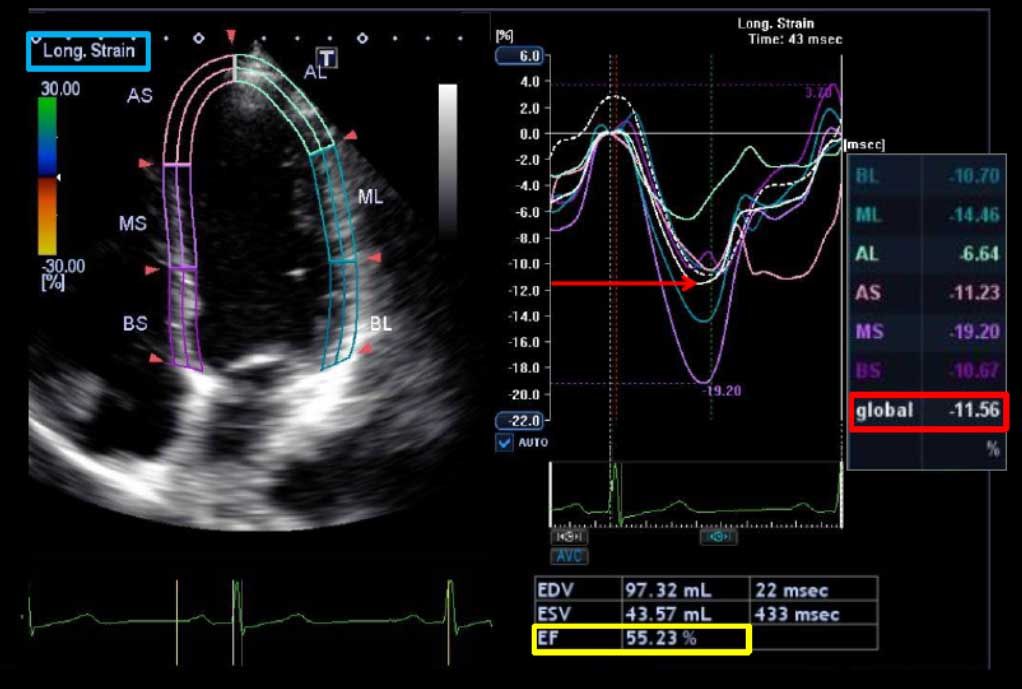
Another noninvasive test is an echocardiogram, known informally as an echo. If you have ever had or seen an ultrasound test used on pregnant women, then the technology and concept of an echo will be familiar to you. With an echo, sound waves are directed at your heart with a device called a transducer that is held on your chest. The sound waves bounce off your heart and are processed electronically to create a video of your heart as it beats.
Not only does an echo show the size and shape of your heart chambers, it also provides information on how well the chambers and valves are functioning or if there is evidence of previous heart damage. y. Clearly, echocardiography offers a great deal of insight into whether structural heart disease is present or if there are problems that could be causing or contributing to AF. The standard echo is also called a transthoracic echocardiogram (TTE), since the pictures are obtained by imaging through the chest wall, or thorax.
Another type of echo is the transesophageal echocardiogram (TEE), which uses a transducer at the end of a tube or probe inserted into the mouth and down the esophagus. This is done because the atria are deep in the chest and not always well imaged with a regular echo. The TEE is especially good at detecting possible clots in the atria. To ease the discomfort of a TEE, the patient is usually sedated and the back of the throat is numbed before the procedure.
Other tests
Your doctor also will order blood tests, primarily to measure thyroid function. Other blood tests may be ordered to evaluate kidney and liver function, mostly to see if there are any limitations with regards to the medications you might require. Additionally, you may have a chest X-ray to get a better assessment of your lungs, especially if there is any suspicion of pneumonia or other lung disease. Some physicians also may order exercise tests, especially if the AF is prolonged or considered permanent, to help determine whether your heart rate is under good control.
If necessary, you may undergo an electrophysiology study. Essentially, electrophysiology is the science of measuring the electrical potential of the body; for example, the electrical activity of the brain can be assessed by an electroencephalogram or EEG. Cardiac electrophysiology usually requires more invasive methods, such as inserting a special cardiac catheter that can record both ongoing electrical activity of the heart as well as responses to specific stimulation of the heart. Such tests help physicians look at a range of complex arrhythmias including AF, provide further insight into the potential causes of abnormal ECGs, assess your risk of developing AF or other heart rhythm problems in the future, and create a treatment plan if you do have AF. The electrophysiology study is not a routine test, and is not performed in all patients with AF. Usually this type of evaluation is reserved for patients who have failed drug treatment and are being considered for ablation therapy (see below).
TREATMENT
Atrial fibrillation can be tough to treat. Management of AF is designed to achieve several objectives:
- Prevent blood clots from forming;
- Control the heart rate, concentrating on how many times per minute the heart beats (rate control);
- Restore the heart to a normal rhythm (rhythm control); this helps the heart’s chambers work together more efficiently, which also can improve rate control;
- Treat underlying conditions that may be causing or worsening the AF, such as overactive thyroid function, other metabolic imbalances or various cardiac diseases.
There are different strategies to treat AF, and the goal may be to achieve some or all of the above objectives. Which approach is best for you will depend on various factors, including whether you are currently being treated for other heart or medical problems. Sometimes you will need a combination of treatments to effectively treat your AF.
Prevention of blood clots
The two most common drugs used to prevent blood clot formation (and thus reduce the risk of stroke) are warfarin and aspirin. Warfarin (commonly known as Coumadin) is more effective than aspirin for preventing stroke in this situation. However, warfarin has more side effects – such as potential bleeding problems – than aspirin. Aspirin is the standard treatment for patients without other risk factors for stroke who are also under 75 years of age. If you have only one moderate risk factor for stroke in addition to atrial fibrillation (such as hypertension, diabetes, or heart failure), either aspirin or warfarin may be considered to reduce stroke risk. If you have at least one high-risk factor (e.g., a previous stroke or TIA, age older than 75), you will likely receive warfarin.
Because warfarin is a powerful blood thinner, it requires intense monitoring. Such monitoring involves regular blood tests to measure INR. INR stands for international normalized ratio and this test allows doctors to determine how thin the blood is. For patients with atrial fibrillation, goal INR is usually 2.0 to 2.5. The frequency of INR measurements varies from patient to patient and is driven by how stable the INR measurements are over time.
While aspirin and warfarin can be very effective in reducing the risk of stroke (and heart attack), they are associated with a small risk of serious side effects. Most of the side effects are bleeding related. Patients at higher risk for injury (those with balance issues, patients who abuse alcohol, and those who work in professions where falls are possible, etc.) may not be able to use warfarin, even if they would otherwise qualify for this therapy.
Rate control
To slow heart rate, doctors usually rely on beta-blockers (such as metoprolol, propranolol, etc.), calcium channel blockers (verapamil, diltiazem, etc.), or digoxin. Other agents can be prescribed depending on your particular needs. Beta blockers and calcium channel blockers, although relatively safe, can lower blood pressure and slow the heart rate profoundly. That is why your doctor will carefully monitor the effects of whatever medication you are prescribed.
Rhythm control
Ideally, you want to get your heart to regain its normal rhythm, although this becomes more difficult the longer you have AF. To convert the heart to normal sinus rhythm, doctors may use cardioversion, which is defined as the conversion of one cardiac rhythm or electrical pattern to another. This can be accomplished with drug therapy or with medical procedures.
The medications used to treat AF, generally referred to as antiarrhythmics, are designed to suppress arrhythmias or pharmacologically convert an arrhythmia to a normal rhythm. The particular agent used to treat an episode of AF will depend on a number of variables, including the type of AF being treated (paroxysmal or persistent), patient age and other health issues which may be present. These drugs may be given by mouth or intravenously for faster delivery (although the latter is more likely if you have been hospitalized). If the antiarrhythmic medications produce the desired effect on an episode of AF (that is, you return to normal sinus rhythm), you may be given the same or similar medication to prevent repeat episodes of AF. In some cases, you will need to take the medicine on a regular, ongoing basis; in others, you will take it as needed.
One potential side effect of medications that are used to control heart rhythm is that they may paradoxically cause different rhythm problems (“proarrhythmic effect”). This is why some of these medications are only administered in a hospital setting and why your doctor will carefully monitor the effects of whatever medication you are prescribed. Ongoing research is evaluating newer agents that may improve on the effectiveness or safety of the currently available antiarrhythmic drugs. It is always wise to periodically check in with your doctor to see if any new medications are available that would be beneficial in your particular case.
Alternatives to drug therapy
When medications do not work, there are alternatives. Electrical cardioversion uses a jolt of electricity to your heart either through paddles or wired patches attached to your chest. This is a controlled, usually prescheduled procedure – not the type of emergency “defibrillation” depicted in film or on TV when a character’s heart has stopped. Defibrillation is done under light anesthesia in the hospital, and the patient usually goes home the day of the procedure.
Another option is catheter ablation, which targets and destroys small areas of cells in the heart thought to be the source of electrical malfunction. In this technique, a catheter is threaded into your heart and radio frequency energy in the form of radio waves is emitted to selectively cauterize the errant heart cells. This procedure usually improves heart function, exercise capacity, and quality of life.
The aim of catheter ablation is to “cure” AF, although that word may be misleading. Most studies which have looked at the outcome of ablation have followed patients for only 5- to 10-years. It’s unknown whether these “cured” patients may once again develop AF.
Not all patients undergoing ablation have their arrhythmia completely eliminated by the procedure. Nevertheless, many such patients sill experience greatly improved heart rate control. The result of ablation may be that drug therapy that failed to control heart rate in the past may be effective once again. Between those patients experiencing an effective “cure” and those who see great improvement following ablation, the overall success rate of this procedure is about 70% to 80%. One important point: if ablation does not provide rhythm control, medications for that problem may remain necessary, as may the need for antithrombotic therapy to prevent blood clot formation. In some cases, implantation of a pacemaker will be recommended.
By the way, these ablation procedures may be repeated in some patients. As many as one-third of all patients end up getting a second procedure, which often proves effective for a year or more.
Another rhythm-control strategy is the Maze procedure, which often requires open heart surgery, because the clinician must make precise, small cuts (or possibly catheter burns) in specific places on the atria. The goal is to create a pattern of scar tissue – which does not conduct electricity – that effectively “walls off” the errantly firing heart tissue, preventing the AF from spreading to the rest of the heart. The procedure’s name comes from the pattern of incisions made in the atria – which look like a child’s maze. Usually, the Maze procedure is only performed when open heart surgery is required for other reasons.
Rate versus rhythm control
The best-case scenario occurs when a treatment provides both effective rate and rhythm control. However, when treatment is not effective or it loses effectiveness over time, there has been a great deal of argument as to which approach is better: rhythm control or rate control. One common approach is to initially target rhythm control with the thought that restoration of normal sinus rhythm will lower the risk of stroke; reduce symptoms; improve exercise tolerance, quality of life, and even survival; and perhaps permit discontinuation of long-term warfarin therapy. Unfortunately, AF is not always responsive to antiarrhythmic therapy. Moreover, these drugs have been known to have serious side effects. That’s why it makes sense to opt for rate-control strategies in some patients, especially given that rate-control drugs are usually much less toxic than antiarrhythmic therapy.
Some researchers have compared the two strategies to see if either presents a survival advantage over the other. In the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) trial involving 4,060 patients with advanced heart disease, there was no significant difference in terms of mortality rates between patients assigned to rate-control therapy and those receiving rhythm-control therapy. However, the rhythm-control group was hospitalized more often and experienced more adverse drug effects than those undergoing rate-control therapy.
A more recent study, the Atrial Fibrillation with Congestive Heart Failure (AF-CHF) study, involved an even sicker population of patients. Again, rhythm-control was no better than rate control in preventing deaths from cardiovascular causes. Because of the greater spectrum of side effects seen with rhythm control, the investigators concluded that rate control should be the first approach in similar patients with advanced heart failure.
As far as which approach is best for you needs to be determined in the context of your overall health situation. Your personal physician is in the best position to advise you in regards to these considerations.
Overall, the presence of AF does not preclude an active life. The disorder is usually controllable with treatment and many people with atrial fibrillation do very well. However, AF tends to become a chronic condition and may come back even with initially successful treatment.
POSSIBLE COMPLICATION
As previously noted, there is an increased risk of stroke in people with AF and the risk is even greater in the presence of other types of heart disease. Persistent and especially permanent AF also leaves individuals susceptible to other cardiac diseases, especially heart failure, and an overall increased risk of dying. In fact, the death rate of patients with AF is about double that of people with normal sinus rhythm.
Because AF results in less efficient heart pumping, this rhythm can also affect quality of life, making it more difficult to handle even routine physical activities. In some patients, the AF is completely asymptomatic, having no effect on general sense of well being or activity levels.
LIVING WITH ATRIAL FIBRILLATION
Always take antiarrhythmic drugs exactly as directed. These drugs work best when they are at constant levels in the blood. To help keep levels constant, take your medicine as directed; do not miss any doses and never take larger or more frequent doses. Don’t stop taking antiarrhythmic drugs without checking first with your physician, because stopping some of these drugs suddenly could lead to serious side effects. If taking medicine at night interferes with sleep, or if it is difficult to remember to take your medicine during the day, check with a health care professional for suggestions.
When you visit your doctor or an emergency room (whether for an AF-related problem or not), bring a detailed list of all your prescription drugs with you. Having a complete picture of all your medications is critical in any health care setting, but it is especially important if you are taking antiarrhythmics. Also, keep all medical appointments; don’t assume that because you’re feeling better it is not necessary to visit your doctor. Precise updates on your condition are required to make sure that the treatment strategy is right (and safe) for you. Keeping regular doctor’s appointments is particularly critical if you are taking anticoagulants or blood-thinning medications. If you experience medication side effects or symptoms of AF, be sure to share that with your doctor.
Besides making sure you follow all directions related to your prescription medications, beware of over-the-counter medicines – those that do not require a prescription – including nutritional supplements and cold and allergy medicines. Some of these widely available drugs may contain stimulants or have other properties that can trigger arrhythmias and/or interact with your prescription medications in ways that can lessen their effectiveness or make the prescription drug much more powerful, increasing the likelihood of a serious side effect or other adverse event.
Limiting alcohol consumption is important, too, especially if alcohol triggers your AF. Reducing intake of caffeinated beverages may also be recommended since caffeine has stimulating properties that could be harmful in people with AF.
PREVENTION
Left untreated, AF causes the atrial chambers to weaken and stretch out. This makes it even harder for the atria to contract properly, which leads to even more blood pooling in the atria, and a greater risk of stroke and heart failure. Treating AF correctly is the best way to reduce stroke risk.
If you are at risk of developing AF (based on family history, for example) you can help prevent AF. This requires action that can prevent or control the major risk factors for AF, such as coronary artery disease, hypertension, excess weight and diabetes. By avoiding these risk factors, you can significantly reduce your chances of experiencing AF during your lifetime.
This requires adopting a heart-healthy lifestyle, which means weight loss if you are overweight, changing to a heart-healthy diet, becoming more physically active, and making sure that hypertension or other conditions that can lead to heart disease are treated and well managed.
**Source: Cardiosource- American College of Cardiology.