β blockers for Heart Failure: Which One Should You Use?
β blockers are a cornerstone of the medical management of heart failure. The long term use of certain β blockers in patients with heart failure reduces hospital admissions and improves symptoms, quality of life, and survival. However, it is still unclear whether this is a class effect or whether one β blocker is superior to another.
Three landmark placebo-controlled trials of nearly 9000 patients with heart failure demonstrated the efficacy of carvedilol, long acting metoprolol succinate, and bisoprolol in reducing mortality and hospital admission in patients with heart failure. However, large trials of nebivolol and bucindolol found no reductions in all-cause mortality compared with placebo, despite benefits in cardiovascular morbidity or mortality (1).
A systematic review and meta-analysis of 8 randomized, controlled, direct-comparison trials involving 4,563 patients with systolic heart failure receiving atenolol, bisoprolol, metoprolol, nebivolol, or carvedilol. In this analysis, carvedilol, as compared against atenolol, bisoprolol, metoprolol and nebivolol in randomized direct comparison trials, significantly reduced all-cause mortality in systolic HF patients (2).
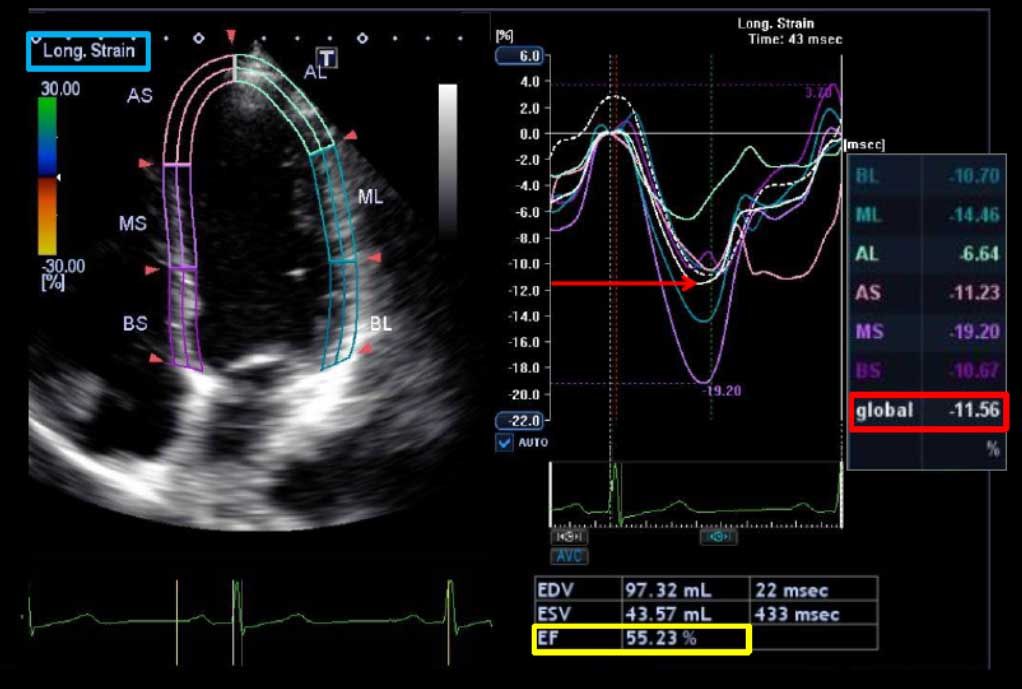
A more recent meta-analysis analyzed the results of 21 randomized trials (focusing on atenolol, bisoprolol, bucindolol, carvedilol, metoprolol, and nebivolol) comparing β blockers with other β blockers or other treatments in patients with heart failure and reduced ejection fraction (3). The primary endpoint was all cause death at the longest available follow-up, assessed with odds ratios and Bayesian random effect 95% credible intervals, with independent extraction by observers. As expected, in the overall analysis, β blockers provided credible mortality benefits in comparison with placebo or standard treatment after a median of 12 months (odds ratio 0.69, 0.56 to 0.80). However, no obvious differences were found when comparing the different β blockers head to head for the risk of death, sudden cardiac death, death due to pump failure, or drug discontinuation. Accordingly, improvements in left ventricular ejection fraction were also similar irrespective of the individual study drug.
CONCLUSION: The benefits of β blockers in patients with heart failure with reduced ejection fraction seem to be mainly due to a class effect, as no statistical evidence from current trials supports the superiority of any single agent over the others. Therefore, β blockers reduce mortality but do not differ from each other.